Rafael S. Beolchi(a), DDS, MSc
Carlos Shimokawa(b), DDS, MSc, PhD
Bruno Pelissier(c), MCU-PhD
(a) University of São Paulo, School of Dentistry, São Paulo, São Paulo, Brazil.
(b) University of São Paulo, School of Dentistry, São Paulo, São Paulo, Brazil.
(c) MCU-PH, Dentisterie Restauratrice, service OCE. UFR d’Odontologie de Montpellier I. 545 Avenue du Pr JL Viala. 34193 Montpellier Cedex 5. Laboratoire EA 4203
Beam Homogeneity
Beam homogeneity is the ability of a curing lamp to deliver a beam of light that is uniform all over its footprint, and it is also another important feature. In the cases when the curing lamp presents more than one wavelength is important that all colors to be spread at once. Also, even lamps that produce only one color may also suffer from lack of beam homogeneity.
Lightcurable composites can be prejudiced by a non-homogeneous light beam profile because they will not be uniformly polymerized at the periphery and may exhibit low bond strength values where they received less radiant exposure. This non-uniformity can generate areas that are well cured, whereas others are poorly cured, all within the same restoration.
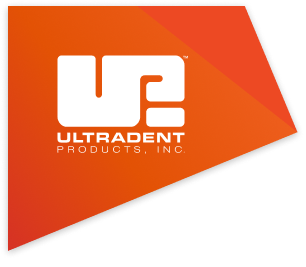
To illustrate this concept, it is possible to go back to Figure 1. It is possible to note the beam profiles from two different lights superimposed over a typical occlusal preparation in a lower first molar. Note that the size of the restoration in relation to the tip diameter on the right needs multiple exposures in order to expose the entire occlusal restoration to an adequate amount of light, and that not only because of the smaller diameter, also because of the lack of homogeneity.
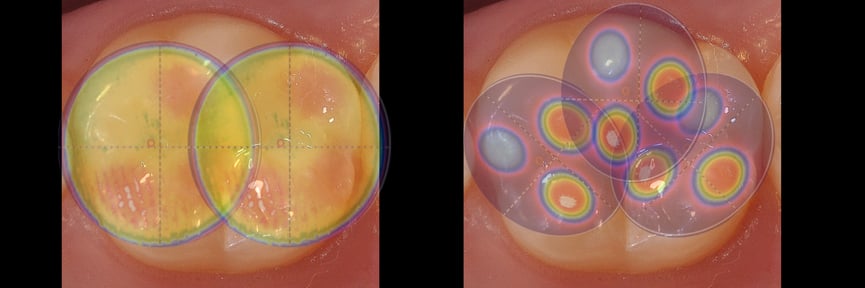
Figure1: Smaller tip diameters requires several applications in order to proper polymerize larger cavities. Also, knowing the beam homogeneity is fundamental to understand how the composite is being cured.
The analysis of the light beam profile may present differences in the light distribution across the LCU tips. This is important information that allows both dentists and researchers to identify “hot spots” of high irradiance and tip areas that emit a low irradiance.
The non-homogeneity of the beam profile can be even more concerning with the introduction of the bulk-fill composites. Since it is now advocated that larger restorations can be made using a single portion of RBC with just one light exposure to bulk cure the entire restoration, the result is that some parts of these restorations may now be photoactivated by areas of the light. However, if the dentist knows that the light output is inhomogeneous, they may choose to use an incremental filling technique and multiple light exposures to reduce the negative effects of the inhomogeneity within the light devices beam profile25.
In cases when a lamp is equipped with a lens, such as VALOTM, it can be noted that all 4 different beams are separated, when the light beam device is observed away from a surface (figure 9a and 9c). Closer to the surface, in a clinical distance, it can be noted that all different colors (wavelengths) are superimposed, thanks to the focal distance provided by the lens (Figure 9b and 9d).
 Figure 9a
Figure 9a
 Figure 9b
Figure 9b
Figure 9 (a, b): 4 different beams seem separated, when the light beam device is observed away from a surface. Closer to the surface, in a clinical distance, all different wavelengths are superimposed.
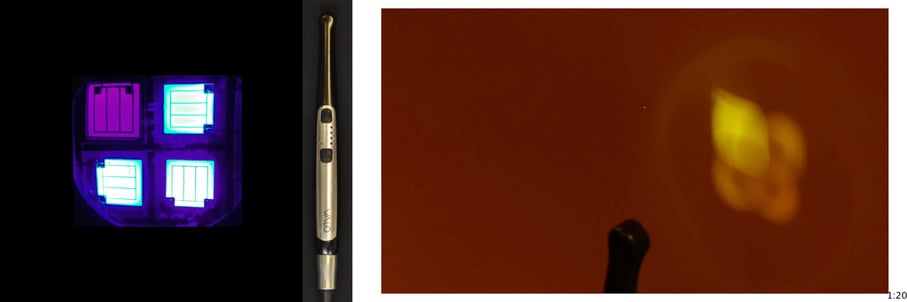 Figure 9c
Figure 9c
 Figure 9d
Figure 9d
Figure 9 (c, d): The images depict the same situation from Figure 9 (a, b), under an orange filter.
To better illustrate this concept, Figure 10 a and b presents the tridimensional representation of the beam profile of the Bluephase Style (Ivoclar) lamp. Figure 10a shows the beam profile when analyzed from 0mm, and figure 10b depicts the same device when measured from 9mm, simulating a clinical distance similar to a regular Class II. Fig. 11c shows a tridimensional view of image 11a (0mm), and 11d the same, but for the image 10b (9mm). Note how there’s a lack of not only homogeneity, but also, no collimation.
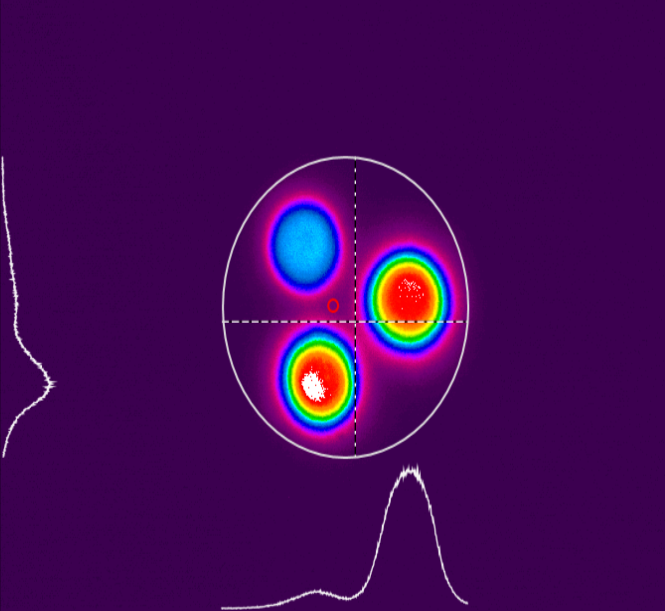
Figure 10a
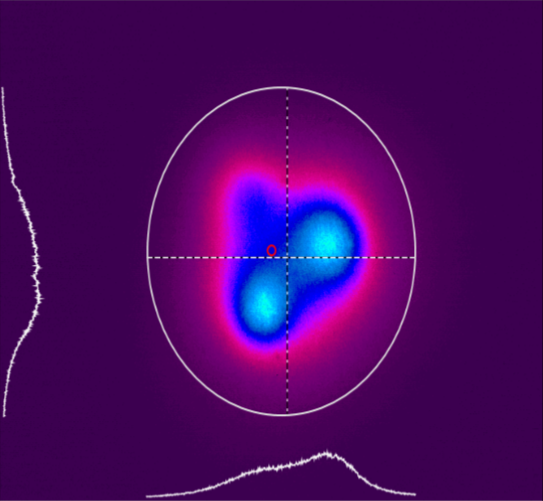
Figure 10b
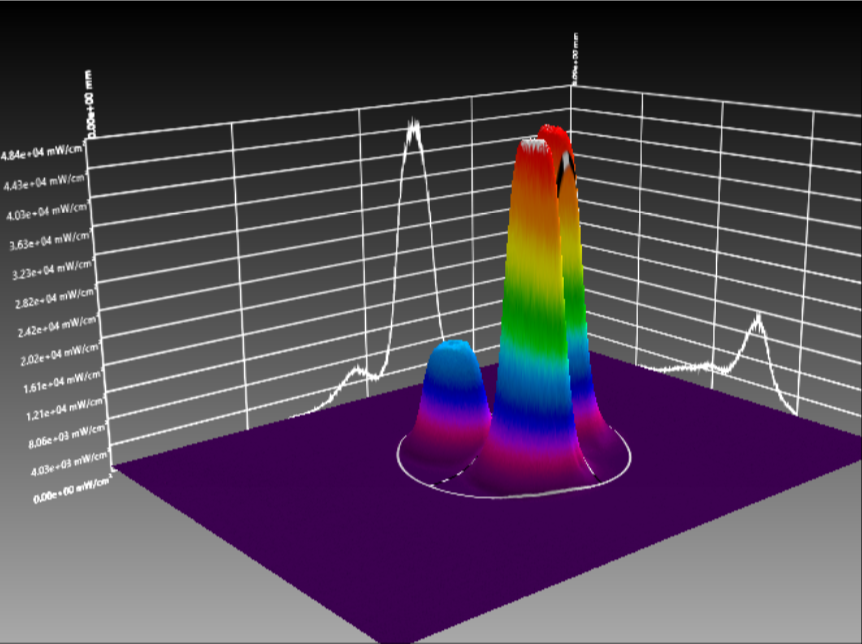
Figure 10c
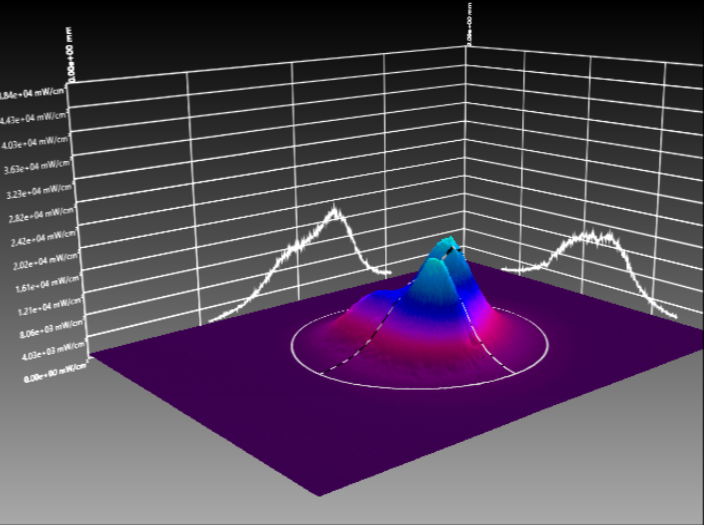
Figure 10d
Figure 10 (a, b, c, d): Tridimensional representation of the beam profile of the Bluephase Style (Ivoclar) lamp. Figure 10a shows the beam profile when analyzed from 0mm, and figure 10b depicts the device measured from 9mm. Fig. 10c shows a tridimensional view at 0mm, and 10d the same, but for 9mm.
Similarly to figure 10, figure 11a and 11 band b also depicts another lamp, now Ultradent's VALO at 0 and 9mm, respectively. It is possible to note that both collimation and beam homogeneity in this case are maintained even when the light is analyzed at 9mm from the sensor, contrary to the other device.
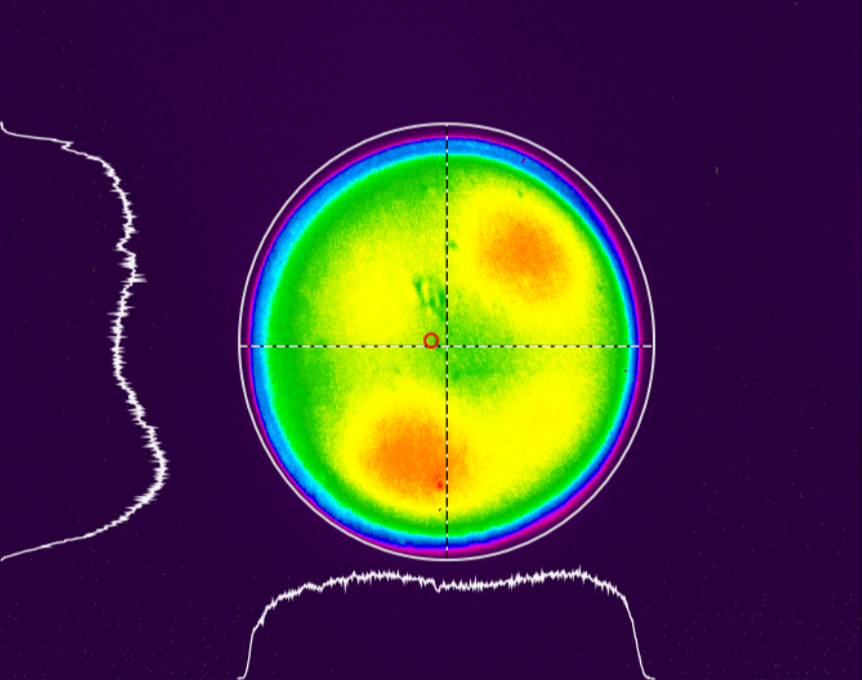 Figure 11a
Figure 11a
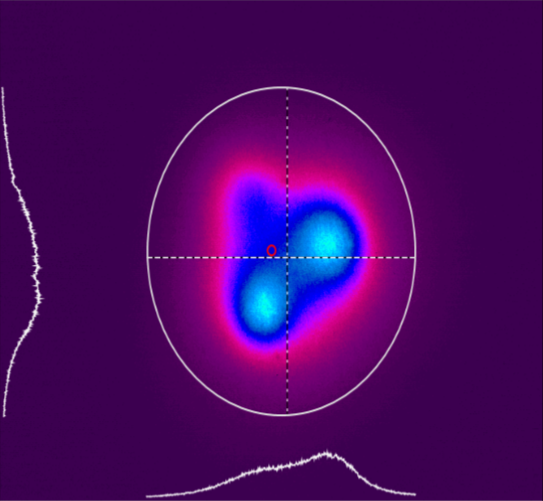
Figure 11b
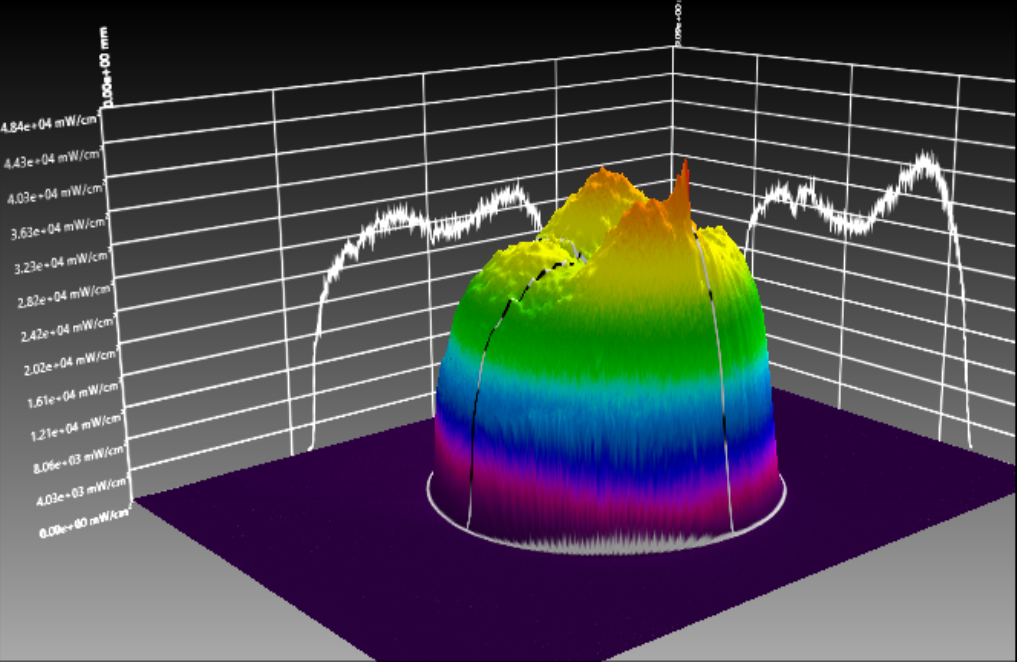 Figure 11c
Figure 11c
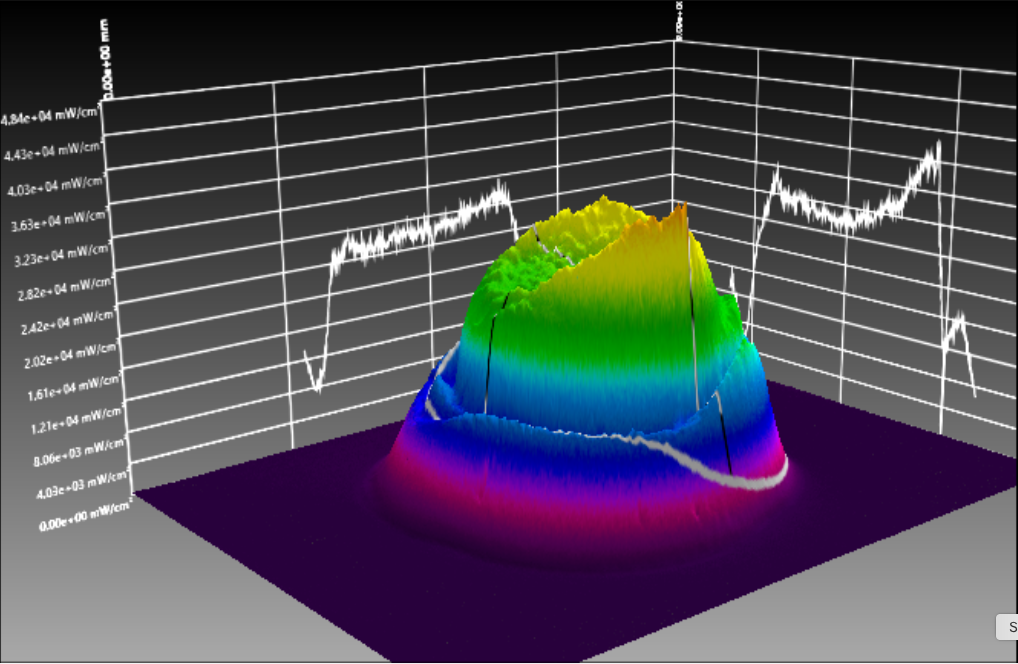 Figure 11d
Figure 11d
Figure 11 (a, b, c, d): Tridimensional representation of the beam profile of the Valo Grand (Ultradent). Figure 11a shows the beam profile when analyzed from 0mm, and figure 11b depicts the device measured from 9mm. Fig. 11c shows a tridimensional view at 0mm, and 11d the same, but for 9mm.
Both the tip diameter and the homogeneity of the light emitted from the lightcuring devices can and will affected the results of proper light polymerization. Results from articles reported less variation in the surface microhardness when the VALOTM Grand was used26, and that’s due to its good homogeneity.
Final remarks
Well-polymerized dental composites present better mechanical properties and, therefore, better clinical performance. This is especially important since dental composite is a demanding material in terms of manipulation, and the mouth itself is an inhospitable environment. When curing a composite, we should not pay attention only to the power output of the curing light, as devices with similar light outputs can present significantly different behavior. Other factors, such as energy density, light collimation, which photoinitiators are being used in the composite, location and type of restoration, distance from light tip to restoration and beam homogeneity must also be taken into account.
Besides all that, it is also important to note that everything that has been discussed here is by taking into account some trivial, but no less important clinical factors, namely:
- That the tip of the light is being held in a stable way, or in other words, that there’s no moving of the tip.
- That the tip of the lamp is being held in a perpendicular way, and also that there’s no obstacle, such as matrixes blocking the path of the light, creating shadowy zones. Remember that light does not make curves, and because of that, the best lights also require a low profile, so they can reach all regions of the mouth.
- Finally, that the tip is pristine clean. Also, that the barrier is properly adapted, with no gaps or seams between the tip and the tooth cavity, as those factors can hinder the light output severely.
This is especially important living in a time of minimally invasive dentistry, where the esthetic demand is already a reality, and the need for restorations to remain beautiful and in place for longer periods of time is mandatory.
References
1 Price, R.B.; McLeod, M. E.; Felix, C. M. Quantifying Light Energy Delivered to a Class I Restoration J Can Dent Assoc 2010; 76:a23
2 Price R.B., Felix C.A. Effect of delivering light in specific narrow bandwidths from 394 to 515nm on the microhardness of resin composites Dental Materials 2009 25(7) 899- 908
3 Rueggeberg FA. State-of-the-art: dental lightcuring - a review. Dent Mater. 2011 Jan;27(1):39-52. Review.
4 Hyun HK, Christoferson CK, Pfeifer CS, Felix C, Ferracane JL. Effect of shade, opacity and layer thickness on light transmission through a nano-hybrid dental composite during curing. J Esthet Restor Dent. 2017 Sep;29(5):362-367. doi: 10.1111/jerd.12311. Epub 2017 Jun 19.
5 Halvorson RH, Erickson RL, Davidson CL. Energy dependent polymerization of resin-based composite. Dent Mater. 2002 Sep;18(6):463-9.
6 Koran P, Kürschner R. Effect of sequential versus continuous irradiation of a lightcured resin composite on shrinkage, viscosity, adhesion, and degree of polymerization. Am J Dent 10, 17–22 (1998)
7 Fróes-Salgado NR, Francci C, Kawano Y. Influência do modo de fotoativação e da distância de irradiação no grau de conversão de um compósito. Perspect Oral Sci 2009 Ago; 1(1):11-17.
8 Kelsey W, Blankenau RJ, Powell GL, Barkmeyer W, Stormberg E. Power and time requirements for using the argon laser to polymerize composite resins. J Clin Laser Med Surg 1992;10:273–8.
9 Benetti AR, Asmussen E, Peutzfeldt A. Influence of curing rate of resin composite on the bond strength to dentin. Oper Dent. 2007 Mar-Apr;32(2):144-8.
10 Pfeifer CS, Ferracane JL, Sakaguchi RL, Braga RR. Photoinitiator content in restorative composites: influence on degree of conversion, reaction kinetics, volumetric shrinkage and polymerization stress. Am J Dent. 2009 Aug;22(4):206-10.
11 Rode KM, Kawano Y, Turbino ML. Evaluation of curing light distance on resin composite microhardness and polymerization. Oper Dent. 2007 Nov-Dec;32(6):571-8.
12 Beolchi RS, Garófalo JC, Forti W, Palo RM. O seu fotopolimerizador está preparado para os novos materiais? Revista APCD de Estética 2013;v.1(3) p. 240-250.
13 Mills RW, Jandt KD, Ashworth SH. Dental composite depth of cure with halogen and blue light emitting diode technology. Br Dent J. 1999 Apr 24;186(8):388-91.
14 Rueggeberg F. Contemporary issues in lightcuring. Comp Cont Educ Dent 1999;20(Suppl. 25):S4–15
15 Rutsch W, Dietliker D, Leppard D, Kohler M, Misev L, Kolczak U. Recent developments in photoinitiators. Prog Org Coat 1996;27:227–39.
16 Lienhard O,inventor. Canrad Precision Industries,Inc., assignee: instrument for transmitting ultra-violet radiation to a limited area. United States Patent 3,712,984; 1973.
17 Neumann MG, Miranda Jr WG, Schmitt CC, Rueggeberg FA, Correa IC. Molar extinction coefficients and the photon absorption efficiency of dental photoinitiators and light curing units. J Dent 2005;33:525–32.
18 Park YJ, Chae KH, Rawls HR. Development of a new photoinitiation system for dental light-cure composite resins. Dent Mater 1999;15:120–7.
19 Palin WM, Leprince JG, Hadis MA Shining a light on high volume photocurable materials. Dent Mater. 2018 May;34(5):695-710.
20 Albuquerque PP, Moreira AD, Moraes RR, Cavalcante LM, Schneider LF. Color stability, conversion, water sorption and solubility of dental composites formulated with different photoinitiator systems. J. Dent. 2012 Dec 8. pii: S0300-5712(12)00322-3.
21 Brandt WC, Gomes-Silva C, Frollini E, Souza-Junior, EJ, Sinhoreti, MAC. Dynamic mechanical thermal analysis of composite resins with CQ and PPD as photo-initiators photoactivated by QTH and LED units. J Mech Behav Biomed Mater 24 (2013) 21–29
22 Krames M. Light-emitting diode technology for solid-state lighting. In: National academy of engineering: US frontiers of engineering symposium. 2009.
23 Uhl A, Sigusch BW, Jandt KD. Second generation LEDs for the polymerization of oral biomaterials. Dent Mater 2004;20:80–7
24 Amaral CM, Peris AR, Ambrosano GM, Pimenta LA. Microleakage and gap formation of resin composite restorations polymerized with different techniques. Am J Dent 2004;17:156–60
25 Shimokawa CA, Turbino ML, Harlow JE, Price HL, Price RB. Light output from six battery operated dental curing lights.
Mater Sci Eng C Mater Biol Appl. 2016 Dec 1;69:1036-42. doi: 10.1016/j.msec.2016.07.033. Epub 2016 Jul 21.
26 Shimokawa CAK, Turbino ML, Giannini M, Braga RR, Price RB. Effect of light curing units on the polymerization of bulk fill resin-based composites Dent Mater. 2018 Aug;34(8):1211-1221. doi: 10.1016/j.dental.2018.05.002. Epub 2018 May 22.