Controlling risk will be a primary concern for dentists while adapting their practices to the changing circumstances due to COVID-19. Prioritizing safety while caring for patients will create new hurdles for day-to-day operations—and knowing how to start implementing the recently required protocols can seem daunting.
Making a set plan will help your practice find its stride while offering the safest environment for you, your staff, and your patients. Dr. Deanna Snitzer, DDS developed a Hierarchy of Controls to assist dentists and their teams in navigating these changes. The chart relies on CDC recommendations and OSHA standards — and Dr. Snitzer adapted them as best practices for dental offices.
The CDC (Centers for Disease Control and Prevention in the USA) is the leading science-based, data-driven, service organization, which aims to protect the public health in the US. Likewise, the OSHA standards represent US specific regulations in terms of health and well-being. They are based on the Occupational Safety and Health Act of 1970 (OSHAct), which was passed to prevent workers from being killed or seriously harmed at work. The law requires that employers provide their employees with working conditions that are free of known dangers.
Dr. Snitzer calls it a starting point, not a one size fits all solution, and she stresses that using your own clinical judgement for what’s best for your practice is the optimal way to create a safe working environment.
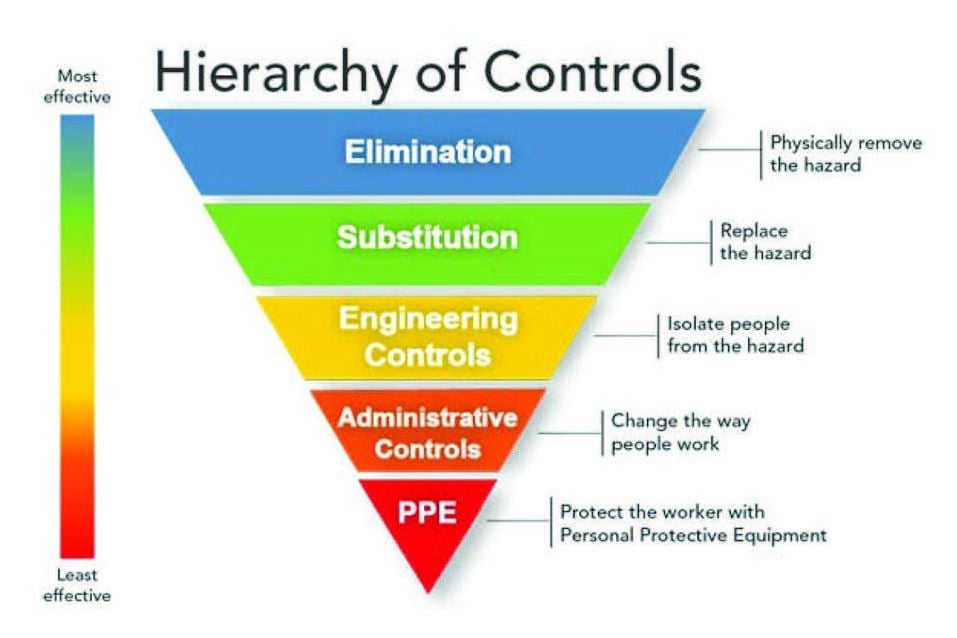
Dr. Snitzer’s Hierarchy of Controls. More information here.
“Patients need to know that their dentist has been researching [safety protocols], that they have a plan and that the whole team is on the same page,” Snitzer continues with “[Dentists] need to get back to work in a very specific, safe manner. It needs to be organized and it needs to be public information and it needs to be across the board so everyone is on the same page.”
Engineering Controls
Keeping your practice as safe as possible is rooted in eliminating risks, but in the case of COVID-19 (or other viruses), it’s impossible to just wave a wand and truly eliminate risk. “We can’t just wish that this virus doesn’t exist, or just erase it from society” Snitzer says. “The document I created focuses on things we can control. The first level of things we can control are engineering controls, trying to keep the risk out, the screening processes.”
Engineering controls include, but are not limited to:
- Pre-screening patients 24 hours before their visit with CDC recommended questions
- Temperature screening of patients before entry to the office
- Not allowing extraneous persons into the office
- Removing magazines and toys from your office to avoid multiple people touching items
- Weather permitting, opening windows and doors to promote airflow
- Adding barriers, such as plexiglass sneeze guards at the front desk
- Regular disinfection of reception desk, waiting rooms, waiting room furniture, door handles, toilets, and other public areas in the practice.
- Single use towels in washing rooms
More than anything, Dr. Snitzer stresses the importance of screening patients. “If the problem isn’t walking in your door, you don’t have to worry about it,” Snitzer says.
Administrative Controls

Day to day processes are changing in response to COVID-19 and many of these shifting processes are considered in Dr. Snitzer’s Hierarchy of Controls. “Maximize our social distancing, maximize barriers between us and our patients, minimize interactions between people [. . . ] These things are challenging, but they’re things we need to do right now.” She recommends using your parking lot as a lobby. “We have patients call or text when they arrive, then our hygienist or assistant goes outside, wearing their proper personal protective equipment (PPE), with a thermometer to additionally screen the patient and make sure they aren’t showing any symptoms.”
“The ideal situation is patients have one or two social interactions [with our staff], maximum.”
Once patients come inside, Dr. Snitzer is having patients immediately wash their hands or use hand sanitizer. “Once they have clean hands, they can be taken directly into the treatment room,” she says. “The ideal situation is patients have one or two social interactions [with our staff], maximum.” She’s also having patients wash their hands/use hand sanitizer when they head out of her office and is stressing clean hands as a priority for her staff. “Use lotion in the evenings or glove-safe lotion during the day to prevent breaks in the skin barrier. Washing hands in view of the patient may help them feel more secure.”
Dr. Snitzer’s office is accepting credit card payments over the phone or checks slipped under the door.
Personal Protective Equipment

Personal Protective Equipment (PPE) has entered the popular lexicon in recent months—while facemasks and other gear are prevalent in public, they’re more necessary than ever for medical professionals.
All quotes from Dr. Snitzer originated from the above conversation with Hartley Lojik from Ultradent Products. You can click here to watch the video.
Masks, gowns, hair cover, goggles, gloves and scrubs are now the new normal. Dr. Snitzer positions these as a “last line of defense” in her Hierarchy of Control.
You can find the ECDC (European Center for Disease Prevention and Control) recommendations for wearing and removing PPE in healthcare settings here.
Click here for Danish version.
Click here for Finnish version.
Click here for Norwegian version.
Click here for Swedish version.
For other Covid-19 related information for dental practices in Denmark you can visit here.
For other Covid-19 related information for dental practices in Finland you can visit here and here.
For other Covid-19 related information for dental practices in Norway you can visit here.
For other Covid-19 related information for dental practices in Sweden you can visit here.